Almost everyone has heard of varicose veins. In most people, this vascular disease is associated with leg problems, but the pelvic organs are often the site of the pathological process. One type of this pathology is uterine varicose veins.
The disease is primarily diagnosed in women or girls who have reached childbearing age, but in some cases it also occurs in adolescent girls. In order to cope with pathology, it is important to understand the main causes and symptoms of its occurrence, as well as thoughts on treatments.
pathological features
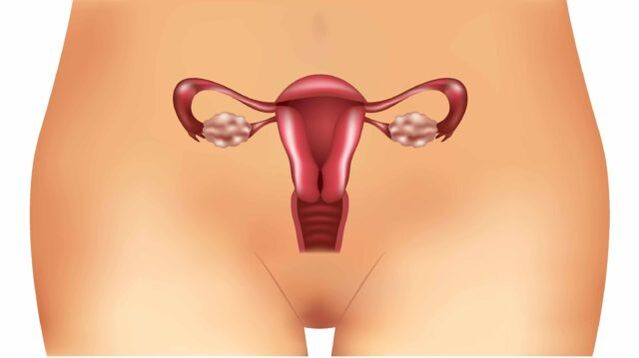
Uterine varicose veins, what is this disease? This medical term refers to diseases caused by a variety of pathological factors affecting the venous network of the pelvic organs:
- Thinning of blood vessel walls.
- Formation of vascular nodules.
- Dilation of the venous lumen.
These three factors negatively affect the blood circulation process in separate parts of the organ and lead to venous valve insufficiency in the same area. The disease is difficult to diagnose due to the lack of overt clinical symptoms and the similarity to inflammatory pelvic organ disease. For these reasons, the pathology is usually detected in the severe stage, when its treatment is much more complicated.
Gynecologists distinguish two subspecies of pathological processes:
- Uterine varicose veins.
- cervical varicose veins.
Regardless, the complications of this disease are dangerous and include inflammatory processes that cover the uterus, ovaries, and vagina. The most serious complication is infertility.
cause of disease
Understanding the underlying factors in disease development provides several key benefits. First, it enables doctors to diagnose faster and more accurately and prescribe appropriate treatment. Second, women will be able to try to stop the pathology from developing.
Consider the most likely causes of uterine varicose veins:
- Pregnancy is considered a major factor in the development of the pathological process. Already in the embryonic stage, then as the fetus grows and develops, the uterine circulation increases (depending a lot on the period). Meanwhile, in vessels with weak vein walls, valve function is disturbed and stretched. In addition, the growing fetus increases the load on the pelvic organs, which may also contribute to the development of the disease.
- Long-term use of hormonal drugs. Certain medications can adversely affect the condition of blood vessels, which lose their elasticity.
- Another factor contributing to the disease is decreased physical activity. A sedentary or sedentary lifestyle can lead to decreased muscle contractions, which can disrupt blood circulation.
- Increase physical activity in the pelvic area. In this case, as during pregnancy, blood flow to the pelvic organs, especially the uterus, increases.
- Increased constipation - In this case, the cause of varicose veins again becomes increased blood flow. However, circulation is now increased due to increased intra-abdominal pressure.
- Congenital abnormalities of uterine structure.
- Artificial termination of pregnancy.
- Dystocia.
- Inflammatory processes in the pelvic organs.
Symptoms and Diagnosis
The complexity of diagnosing uterine varicose veins is that the symptoms of this disease are masked by other pathologies. In addition, the clinical manifestations that indicate the development of the disease are rather poor:
- Lower abdominal pain is frequent, recurring more than 3-4 times a week, closer to the pubic area. The pain syndrome is obvious, the nature of the pain is pulling and aching. In some cases, the pain was so severe that women lost their ability to work and even had trouble getting out of bed.
- More than 80% of women with varicose veins experience discomfort or even pain during or after sex.
- Violation of the menstrual cycle, delays in menstruation for up to 50-60 days are possible. In this case, the discharge is usually minimal and the menstrual duration is prolonged by 5-7 days. Many women go without a period for a long time, which is considered the first sign of menopause.
This clinical presentation is inherent in many other gynecological disorders. For this reason, it is not possible to make a diagnosis based on symptoms alone, and the doctor is obliged to develop some diagnostic measures. Also, in cervical varicose veins, the symptoms are about the same.
Important note: Uterine varicose veins are mostly diagnosed in the second stage, because it is at this time that the symptoms described begin to upset women. The earlier the pathology is detected and treatment is started, the lower the chances of complications, especially infertility.
As for the studies of direct assignment, they are as follows:
- Ultrasound, performed by a transvaginal method.
- CT of pelvic organs.
- Doppler imaging.
- Selective oophorography.
The need for each diagnostic method depends on the data obtained as a result of ultrasound because it is performed first.
Features of illness during pregnancy
During pregnancy, the chances of developing uterine varicose veins increase due to the increased load on the entire body and pelvic organs. The disease is incurable until a woman gives birth.

Pathologies that occur during pregnancy influence the choice of mode of delivery. Many times, doctors decide to perform a caesarean section. This is done to avoid complications such as thrombophlebitis, internal bleeding, and thrombosis.
No matter what stage of pregnancy the disease is detected at, doctors need to constantly monitor the woman to monitor the condition of the fetus and the progression of varicose veins.
IMPORTANT: When planning a pregnancy, get tested to identify varicose veins and other gynecological problems. This will help avoid complications during labor and reduce the risk of abnormal fetal development.
treatment of disease
To get qualified help for varicose veins, you will need to contact a doctor, first a gynecologist, who will then refer you to a phlebologist.
The basis of treatment is medication, including the administration of:
- Venotonics - this group of drugs is beneficial for the vascular state. They regulate capillaries and blood vessels, reducing their permeability, increasing elasticity and strengthening the walls of veins.
- Medications that reduce blood viscosity - help improve the inflow and outflow of blood in the affected blood vessels, reducing the likelihood of blood clots forming. The methods of this group are contraindicated in the pathology of the cardiac system.
IMPORTANT: Any medication can only be prescribed by a physician based on the initial diagnosis, the patient's medical history, and taking into account the stage of development of the disease. It is important to note the special care given to women in power.
treatment method
In addition to pharmacological treatment for complete treatment, it is important to have a comprehensive approach and implement the following recommendations:
- follow a sleep regimen;
- Minimize physical activity while maintaining mobility;
- follow a diet high in vegetables, fruits, and oils rich in vitamin E;
- supportive exercise, therapeutic gymnastics;
- Complete exclusion of any bad habits;
- Some doctors recommend doing Kegel exercises, which help strengthen the vaginal muscles.
Surgical treatment
Such drastic measures are required in cases where conservative treatment has not yielded adequate results or the disease has been detected at a late stage. The following surgical interventions are the most popular:
- Phlebectomy is the removal of a single part of a small blood vessel.
- Laser coagulation is the least labor-intensive type of restoring normal blood flow.
- Sclerotherapy is the introduction of an agent that promotes its adhesion into the venous lumen. A lack of blood supply in the blood vessels will lead to its spontaneous elimination.
- In the most severe cases, it is necessary to completely remove the uterus, sometimes together with the appendages.
Ethnoscience
An alternative approach is one of the options for complex treatment in a conservative manner. They are not a complete replacement for medical treatment, but generally affect the success of treatment.
The most effective means of traditional medicine are:
- Horse chestnut infusion: Take 100 grams of chestnut fruit and chop it with the skin. Pour the resulting ingredients into a measure of vodka so that it covers the crushed fruit by 4-5 mm. Hold for 14-15 days in a dark place. After that, infuse 10 drops twice a day. The tool strengthens the walls of blood vessels and thins the blood.
- Clove tincture: 0. 5 liters of vodka, you need to take 100 grams of cloves and 30 grams of propolis. Pour all ingredients into vodka and leave in a dark place for 30 days (need to shake every 2-3 days). Then filter the tincture and take 15ml 3 times a day before meals.
Remember, you should consult your doctor before using the most harmless traditional medicines.
Complications of the disease
The complications of uterine varicose veins can be dangerous without proper treatment. These complications are as follows:
- internal bleeding;
- thrombosis;
- Inflammatory processes in the reproductive organs;
- irregular menstruation;
- ovarian hormonal dysfunction;
- Infertility.
Precaution
Preventing a disease, preventing its progression, is always better than dealing with it or its consequences later. To prevent uterine varicose veins, follow these simple guidelines:
- Leading a mobile lifestyle, walking more and more;
- do gymnastics;
- Eat healthy food, less greasy, fried, spicy, spicy, sour;
- See your gynecologist regularly, especially for the mildest complaints.

Despite the difficulty in detecting uterine varicose veins, to avoid disease progression and complications, consult your doctor if you develop the symptoms described earlier. It is also important to remember that self-treatment is contraindicated in this case, and careful diagnosis and continuous monitoring by a gynecologist and phlebologist are necessary.












































