Varicose veins in the legs (Varicose veins - commonly known as) - externally visible enlargement of the saphenous vein, which develops as a result of varicose veins or post-thrombotic syndrome and is accompanied by a sharp invasion of the venous outflow of the lower extremities.
Modern methods allow radical treatment of varicose veins without incisions and pain.
Varicose Vein Complaint

For many people, varicose veins and spider veins are just a cosmetic concern. In other cases, varicose veins can cause pain and discomfort. Sometimes varicose veins can lead to more serious problems and complications - the appearance of thrombophlebitis or trophic ulcers. Treatment involves removing or closing the deformed vein, which is the job of a phlebologist.
Varicose veins are complete degeneration of the vein wall, associated with weakening of connective tissue (varicose veins of the lower extremities), or severe violation of venous outflow due to venous obstruction or overflow.
Causes of varicose veins in the lower extremities
Varicose veins of lower extremities
The disease is the cause of varicose veins in the legs and occurs in 20-40% of the population in developed countries around the world. Varicose veins have long been a cosmetic defect, but progression of the disease can lead to pain, swelling of the feet and legs, and, in later stages, darkening of the skin on the legs, inflammatory changes and varicose trophic ulcers.
Genetic susceptibility is the main cause of primary varicose veins, however, the disease develops with excessive pressure on the veins. The triggers for varicose veins in the lower extremities are intense physical overwork, pregnancy, and childbirth. In this condition, the venous pressure in the lower extremities increases dramatically and damages the valve device, triggering the mechanism by which the disease develops.
post-thrombotic phlebitis
Secondary varicose veins develop after venous thrombosis or due to congenital diseases (arteriovenous fistula, congenital venous dysplasia). Postthrombotic lesions are complex and progressive pathological processes in the venous system of the lower extremities. The saphenous vein dilates as it fills with blood due to insufficiency or blockage of the deep vein valves. Another cause may be a congenital or acquired arteriovenous fistula. Occasionally, congenital deep vein occlusion, resulting in secondary varicose veins (Klippel-Trenaunay syndrome).
Complications of varicose veins
More than 40% of women and 20% of men have swollen, dilated varicose veins. In 20% of cases, varicose veins lead to trophic ulcers, and more than 25% of patients have varicose vein thrombophlebitis. These complications often require serious treatment and pose a great threat to health.
chronic venous insufficiency

Obstruction of the venous outflow tract results in a pathological condition called chronic venous insufficiency. At the onset of the disease, the appearance of individual nodules with dilated veins can be noticed, which is not of much concern, although they are sometimes painful. Subsequently, the number of varicose veins increases. The disease progresses slowly but steadily. If the first varicose veins appear below the knee, the rate of progression of the disease is much higher. If the disease does not stop, the third stage of venous insufficiency develops gradually. Edema becomes permanent, dark skin develops in the ankle area, and the heaviness in the legs is constantly worrying, which persists even after a night of rest. Thrombophlebitis and skin inflammation, eczema, and dermatitis often develop into varicose veins. The final stage in the development of varicose veins is the appearance of trophic ulcers.
Varicose vein thrombophlebitis

Thrombophlebitis is the most common complication of varicose veins. Thrombophlebitis is inflammation of the vein wall, forming a blood clot in the vein lumen. Thrombophlebitis occurs in both superficial and deep veins. For varicose veins, thrombophlebitis occurs in 25% of patients and is usually superficial. Varicose vein thrombophlebitis is caused by very slow blood flow, especially in large lymph nodes. In these cases, any factor that increases blood clotting (pregnancy, overheating, trauma, sprains, hypothermia and scratches, acute respiratory infections) can contribute to varicose vein thrombosis and its inflammation. Thrombophlebitis with lower extremity varicose veins occurs in 25% of patients. Thrombophlebitis is caused by slowed blood flow in the varicose veins. Thrombophlebitis can progress and lead to deep vein thrombosis. Chronic venous insufficiency is a painful condition that accompanies venous outflow from varicose veins. It is characterized by edema, darkening of the skin, trophic ulcers, and varicose dermatitis.
varicose trophic ulcer

Nutritional ulcers are a hallmark of severe chronic venous insufficiency. This is a long-term non-healing wound that occurs when the venous outflow through the deep and superficial veins is severely disrupted. It occurs in 1% of the general population and 20% of patients with venous disease. Sooner or later every five patients with untreated varicose veins will develop a trophic ulcer. It can develop along with varicose veins and secondary varicose veins. Varicose trophic ulcers do not heal or keep recurring if the pathological venous secretions are not eliminated. Most patients develop trophic ulcers with varicose veins and cause severe distress. Modern minimally invasive methods allow you to reliably remove varicose trophic ulcers without incisions and pain.
Venous Thrombosis and Thromboembolism
Pulmonary embolism is a serious complication of venous thrombosis. Varicose veins are an important risk factor for thrombophlebitis and deep vein thrombosis. Thromboembolism leads to the development of severe heart failure and respiratory failure, with a mortality rate of more than 50%.
Prevention of varicose veins of lower extremities
Any modern person should know what leg varicose veins are and how to treat and prevent them from happening. For genetic predisposition, factors that cause varicose veins should be avoided. Shows the use of intravenous medications, wearing compression stockings during exercise, regular visits by a phlebologist, and intravenous ultrasonography.
Class 1 compression stockings must be used during work, therapeutic exercise, outdoor activities, medical socks for walking for at least 1 hour per day, foot massage, and swimming when working in concomitant conditions. Refuse to use oral contraceptives with complex varicose vein inheritance. Following these simple rules is better than treating varicose veins in the legs.
Avoid factors in strenuous manual labor. For this reason, compression stockings are necessary, especially for those who are prone to varicose veins. Medical knitwear is suitable for all pregnant women, if there is a tendency for varicose veins and thrombophlebitis, wear special compression stockings during labor. It is recommended that all pregnant women see a phlebologist and undergo a venous ultrasound during the last few weeks of pregnancy. This will help reduce the risk of problems with the venous system.
How to treat varicose veins in the legs
Over the past 10 years, the "barbaric" approach to treating varicose veins is becoming a thing of the past, thanks to the emergence of gentler and more effective methods that have been used successfully in the clinic.
sclerotherapy for varicose veins

Sclerotherapy is the introduction of drugs into the lumen of the varicose veins so that the walls "glue" together while the veins disappear. For sclerotherapy, many chemicals are used, and treatment with ozone has been tried. The advent of foam sclerotherapy once revolutionized phlebology. For the first time, there is an effective way to treat varicose veins without major surgery. Currently, foam sclerotherapy is used to remove medium-diameter varicose veins after laser ablation of pathological venous secretions. Sclerotherapy is essential in the treatment of spider veins and reticular varicose veins, and it has no real competition.
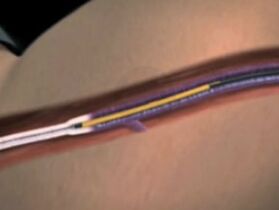
Treating varicose veins with lasers

Varicose veins laser therapy (EVLT) of the lower extremity is the most modern, thorough and cheapest treatment for both treating leg varicose veins and eliminating the cause of trophic ulcers. The point of laser treatment is to heat the vein walls from the inside, and then reabsorb the varicose veins. The latest in EVLT is the 1470 nm laser and radial light guide, introduced into medical practice by phlebologists. The postoperative period following this technique was completely painless and the results were superior to other treatment options - laser intervention was at least 98% curative.
surgical removal of varicose veins

Surgical treatment of varicose veins by removing the main vein trunk is a thing of the past. The risk of complications from dry vein resection forced phlebologists to look for other methods, which led to the development of laser techniques and other methods of venous thermal occlusion. However, according to Müller and Varadi, modifying the classic phlebectomy to a venule resection provides a perfect combination of laser treatment and removal of large varicose veins by puncture without the need for incisions or sutures. Varady's technique saves patients from painful sclerotherapy for large varicose veins. Veneectomy can treat both leg varicose veins and remove varicose veins that are visible anywhere on the body.
radiofrequency ablation of varicose veins
Radiofrequency occlusion (RFO) for leg varicose veins is a modern and safe treatment. The method is based on the use of microwaves to heat a metal probe, which is already the vein wall and causes destruction of the intima. In terms of its painlessness, this method corresponds to laser coagulation with a wavelength of 1470 nm, which is simple to operate and less postoperative pain. However, in terms of long-term therapeutic effects, RFO is far inferior to laser. The effectiveness of RFO is 85% without recurrence. This method is not suitable for the treatment of perforating veins.
Massage and bath for varicose veins

Massage is an active treatment for varicose veins.
Use all types of modern massage, especially in pathologies of the lymphatic and venous system. One of the unique methods is the wrapping lymphatic drainage massage technique, which is very effective in relieving chronic venous insufficiency.
In chronic venous insufficiency, massage is used to relieve venous hypertension in varicose veins and post-thrombotic syndrome. This combination of massage and dressing allows you to effectively eliminate all clinical manifestations of the disease.
Bathing with varicose veins, thrombophlebitis, or post-thrombotic disease can be very dangerous. Any heat stress can trigger the formation of deep vein thrombosis, with all its attendant consequences.
Unfortunately, it is impossible to completely cure varicose veins without eliminating venous secretions and varicose veins. Although with the help of modern treatments it is quite possible to reduce the symptoms associated with venous blood stasis in the legs. However, the prevalence of varicose veins and chronic venous insufficiency has sometimes led to speculation about the problem. Consider modern treatments and fooling methods.
Medications to treat varicose veins
The goals of drug therapy for venous lesions are to reduce symptoms and prevent complications, but these goals are not easy to achieve. Today, the abundance of available means raises another question: which one to choose? Unfortunately, despite theoretically sound use of stopgap measures, most of the proposed drugs are rather inefficient. This is due to a variety of reasons, chief among them the low absorption rate of the medicinal substances of these drugs by the body. An ideal drug for the treatment of venous insufficiency should affect as many of the pathogenic links of chronic venous insufficiency as possible, while having the fewest side effects and a high absorption rate in the human body. There are quite a few snake venoms on the modern medical market. However, they have similar medicinal substances (plant flavonoids), so the effectiveness of one or the other depends only on the concentration and digestibility of the active ingredient.
You shouldn't expect the varicose veins to go away with these medications, however, the lightness in the legs, the reduction of edema, and the disappearance of nighttime cramps can.
creams and gels for varicose veins
While sellers and manufacturers advocate high efficiency, creams and gels don't relieve varicose veins, and varicose veins don't go away. In the initial stages of venous insufficiency, phlebologists do not object to the use of these agents because their friction promotes venous outflow, like a gentle massage, and has a calming effect on the skin. For advanced forms of venous insufficiency, these creams and ointments can be very harmful because of dermatitis and hypersensitivity. Some drugs are used in the development of acute thrombophlebitis and help to subside the inflammatory process, but varicose veins do not disappear from it. Shamanic products containing leeches are popular among the people thanks to just the right advertising, but they have no attitude towards medicines or even leeches, and it doesn't make sense to have high hopes for them.
Medications to treat varicose vein thrombosis
A common complication of varicose veins is thrombophlebitis, especially during pregnancy and the postpartum period. A proven antithrombotic drug is a low-molecular-weight acidic sulfur-containing glycosaminoglycan. For the prevention of thrombophlebitis after varicose vein treatment, tablets are used clinically. They are taken 7 days after laser or radio frequency intervention.
Varicose compression stockings

Compression stockings are undoubtedly one of the most effective means of treating venous edema and reducing the degree of chronic venous insufficiency. Invented over 100 years ago, compression stockings and stockings have become more popular in the 20th century and more in the 21st century and have become an integral part of phlebologists' treatments. This is because it has the following effects:
- Improve venous and lymphatic outflow of the lower extremities,
- improve microcirculation,
- slow the progression of the disease,
- Prevention of varicose vein complications (varicose phlebitis, nutritional disorders),
- Prevention of deep vein thrombosis.
How to use compression stockings
So if you suffer from varicose veins and plan to treat them, you will undoubtedly use compression stockings for days or months (alone) during treatment. If you have swollen feet after get off work and suffer from heavy leg syndrome, you can also use compression stockings during the day to avoid these symptoms at night. If you have untreated varicose vein complications - trophic ulcers or thrombophlebitis - of course, you also use compression to improve the condition of your legs and reduce unpleasant symptoms.
The truth is that compression stockings are promoting the return of venous blood from the legs every second they are worn by improving venous outflow, which is certainly not easy for veins damaged by disease and the law of gravity. Compression sweaters can be called one of mankind's ingenious inventions, but to make it work for you, a few conditions must be met:
- Compressed knitwear is individually selected (according to standard). The main requirement is to conform to the anatomical contours of the limb and, therefore, create the correct pressure gradient.
- Knitwear is individually selected by the doctor (phlebologist). Medical products are marked in mmHg and are classified into compression classes 1, 2, 3, and 4. Each compression level corresponds to a certain pressure. Appropriate compression levels are used at different stages of varicose veins or chronic venous insufficiency. That's why only doctors have the right to prescribe and choose the right compression stockings - taking into account the nature of the pathology and according to individual criteria.
- It should be medical, not slimming knitwear. Only verified brands with RAL certificate.
When do varicose veins need a sweater?
- Correcting "heavy legs" syndrome: reducing severity, edema, improving quality of life;
- During treatment with a phlebologist: after surgery or for a period specified by the specialist;
- slow the progression of varicose veins;
- For the treatment of varicose vein complications (variceal thrombophlebitis).
An essential component of any treatment for varicose veins and chronic venous insufficiency is medical elastic compression. Thanks to compression therapy, swelling and heaviness in the legs can be completely eliminated and conditions are created for a radical treatment of varicose veins of any type. Modern medical knitwear has a high therapeutic effect and excellent aesthetic properties.
elastic bandage |
therapeutic sweatshirt |
|---|---|
The creation of the necessary pressure depends on the technique and skill of the doctor or patient in dressing |
Process curves and pressure levels specified during manufacturing according to compression rating |
Requires medical involvement in bandage application or patient education |
Physician involvement is limited to selection of compression level and product type |
Difficulty providing compression and immobilization in the thigh |
Provides effective compression and immobilization on the thigh |
for non-standard limb shapes |
Limb shape is non-standard and can be customized |
Daily washing can cause the bandage to wear out quickly |
Daily cleaning is necessary to maintain compression performance |
Needs to be replaced after multiple washes |
Guaranteed compression performance for 6 months |
May violate the skin's water and temperature balance |
Porous binding provides skin's normal temperature and moisture balance |
Low aesthetics for convenience and comfort |
High aesthetic properties for ease of use and comfort |
Exercise and exercise for varicose veins
Strength and athletics for varicose veins can be performed after varicose vein syndrome has been eliminated, or with grade 2-3 compression stockings. Modern treatments are able to normalize the varicose legs, removing all limitations.
We draw your attention to comprehensive treatment and prevention exercises developed by leading experts. Its regular implementation will help reduce the manifestations of venous insufficiency of the lower extremities, slow the progression of the disease and reduce the risk of life-threatening complications.
- Leg vein unloading. Breathe deeply and evenly, lie down, close your eyes, and relax. At the same time, place a few pillows under your feet so that they are raised at an angle of 15-20°
- bicycle exercise. Lie on your back, breathe evenly, and imagine that you are riding a bike.
- The exercise consists of several parts, which are performed slowly and smoothly. Lie on your back with your legs straight and breathe deeply. Exhale, bend your right leg and bring your knee to your chest. Inhale, straighten your legs straight up. Exhale and lower. Repeat this exercise alternately with each leg.
- Lie on your back with your arms along your body and your legs straight up. Rotate both feet inwards and then outwards at the same time.
- Alternately bend and straighten your feet back and forth at the ankle joint.
- Alternately bend and straighten your toes.
- Standing position: Legs together, arms along torso. After taking a deep breath, stand on tiptoe, exhale, and return to the starting position.
- Walk without lifting your socks off the floor.
- Vertical scissors. Lie on your back, arms along your body, breathing evenly, legs alternately crossed, alternating.
- Lie on your back, bend your knees, don't lift your feet off the floor. Put your hands on your hips. Inhale slowly and lift your head and torso. At the same time, slide your hands toward your knees. Exhale slowly and return to the starting position.
- Lie on your back with your arms along your body, your legs at a 15-20° angle, and a small pillow between your feet. Inhale slowly, bend over, and tear your hips off the mattress. Exhale slowly and return to the starting position.
- Lie on your back with your arms on your body, bend your knees, and keep your feet on the floor. Breathe out slowly, contract your belly. Inhale slowly to inflate your stomach.
- Lie on your back with your legs elevated 15-20°. Bend your right leg and bring your knee to your chest. At the same time, clasp your feet tightly with your hands. Slowly straighten your legs. Grasp the leg tightly with both hands and slide it along the calf to knee level. Slowly lower your legs and slide your hands over your thighs. Repeat the exercise with the other leg.
- Stand with feet together, arms along your body, inhale slowly, bring your shoulders back, exhale slowly, relax your shoulders, and tilt your head forward.
- Contrasting shower on the legs. Alternate jets of warm and cold water with hard jets. 5-10 minutes per leg.












































